GM case-5
August 21,2022
Case scenario.......
Hi, I am P.kathyayani, 3rd sem medical student.This is an online elog book to discuss our patients health data after taking her consent.This also reflects my patient centered online learning portfolio.
CASE SHEET:40 years male patient from velmakannane admitted at 9:30am in Kim's with fever
Chief complaints:fever since 3 days, weakness since 5 days,nause and vomitting
HISTORY OF PRESENT ILLNESS:
high grade intermittent fever associated with chills since 3 days, generalised weakness since 5 days,frontal headache,nause,stomach abset,no appetite, dry cough since 2 days
ASSOCIATED DISEASES:
Not associated with hypertension, diabetes
PAST HISTORY:
He took medication for 2 days in local hospital for fever which was diagnosed as Typhoid.
He developed allergic reactions over hands and chest ,again medicated for this allergies reactions.
Right hand fracture 5 years ago
PERSONAL HISTORY:
Married
Diet:mixed
Occupation: business
Micturition:normal
Bowels: regular
Allergies:once developed due to medication
addictions :alcohol occasional
FAMILY HISTORY:nil
DRUG HISTORY:
GENERAL EXAMINATION:
No pallor
No clubbings of fingers
No cyanosis
No icterus
No oedema of feet
No lymphadenopathy
No dehydration
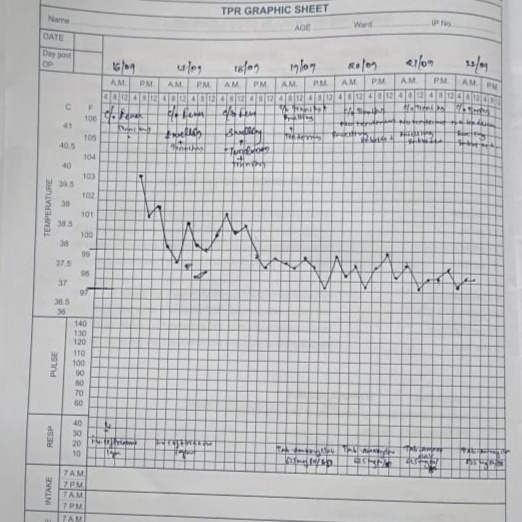
VITALS:
Temperature: 99.6 F
Pulse:92 beats per minute
Respiratory rate: 18 cycles per minute
Blood pressure: 110/70 mm of Hg
SPO2: 98%
GRBS:116 mg%
SYSTEMIC EXAMINATION:
Cardiovascular system:
No thrills
No murumurs
Cardiac sounds: S1, S2
Respiratory system:
No dyspnea
No wheezing
Breath sounds heard: vesicular
Abdomen:
Shape: scaphoid
No tenderness
No palpable mass
Non palpable liver
palpable spleen: splenomegaly
No bruits
Bowel sounds: heard
Central Nervous System:
Conscious
Speech: normal
INVESTIGATIONS:
Microbiology investigations:
PROVISIONAL DIAGNOSIS:
Dengue with thrombocytopenia