GM case 12. 16/9/2023 29 year old female with SOB
Hi, I am P.Kathyayani, 5th sem medical student. This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout this piece of work whatsoever.
CHIEF COMPLAINTS
A 29yr old female patient came to general medicine opd with cheif complaints of SOB since 3days.
HISTORY OF PRESENTING ILLNESS
Patient was apparently aymptomatic till november 2022 . Then she had loss of hair and patches are developed.
Bilatera Pedal edema is present which is of pitting type.
Then she developed shortness of breath which is insidious in onset and gradually progressive in nature.
Renal biopsy was done and diagnosed with lupus nephritis and was on conservative management.
Patient was initially on hemodialysis since feb 2023
DAILY ROUTINE:
Before she got sick, she used to wake up at 5am every morning, cook for her and her husband, take a bath at 6.30am, wash clothes and dishes by 8am, eat breakfast of rice and curry and leave for work by 8.30am. She is a daily wage laborer by occupation and she used to pack lunch which was the same rice and curry as breakfast and eat it at her workplace. She used to reach home by 7 or 8pm after which she would cook dinner of rice and curry, eat and sleep by 11pm.
After she got sick, she stopped going to work and stayed at home, following which she was admitted into the hospital.
HISTORY OF PAST ILLNESS:
He is a k/c/o HTN sicne feb 2023
Not a k/c/o DM,CVA,CVD,TB,Epilepsy,Asthma.
TREATMENT HISTORY:
k/c/o HTN and on medication since feb 2023
Not a k/c/o CAD,TB,asthma,chemo,radiation.
Not a K/C/O blood transfusion (prbc-packed red blood cells).
PERSONAL HISTORY:
Mixed diet
Appetite Lost
Sleep adequate
Bowel movements regular.
Micturition normal.
No addictions
FAMILY HISTORY:
Not significant
PHYSICAL EXAMINATION:
Temp- 98.4 f
BP-150/80 mm hg
Pulse rate-74/min
Respiratory rate-19/min
Spo2-96%
GRBS- 102mg.
-No signs of pallor,cyanosis,lymphadenopathy,icterus.
-bilateral pedal edema present
SYSTEMIC EXAMINATION :
•S1, S2 heard
RESPIRATORY SYSTEM:
•NVBS heard
•Position of trachea - central
•Breath sounds - vesicular
ABDOMEN
•Shape - schaphoid
•No Tenderness
•No palpable mass
-No fluid present.
-No palpable liver or spleen
CENTRAL NERVOUS SYSTEM:
•Intact
•No focal defect
•No abnormality detected
CEREBRAL SIGNS
• No finger nose incordination
•No knee heel incordination.
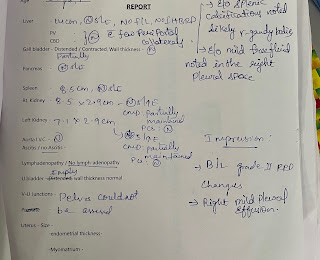
INVESTIGATIONS:
PROVISONAL DIAGNOSIS:
CKD on MHD with k/c/o Hypertension
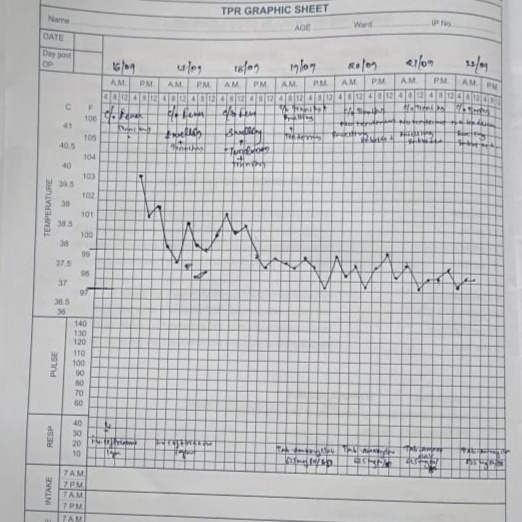
TREATMENT:
1.Fluid restriction <5L per day
2.Salt restriction <2gms per day
3.T.Nicardia 30mg po/bd
4. Tab predinisolone 5mg po/bd
5. Tab arkamime 0.1mg po/tid
6.Tab Shelcal-ct po/od
7.T NODOSIS 500mg po/bd
8. Monitor vitals 4th hourly
9. Inform SOS