GM Case 9 13/09/2023 -58 year female with headache since 2 months
Hi I am P.Kathyayani, 5th sem medical student. This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout this piece of work whatever.
CHIEF COMPLAINTS:
58 year old female, resident of Suryapet, daily wage laborer by occupation came to OPD with chief complaints of headache since 2 months.
HISTORY OF PRESENT ILLNESS:
H/o trauma to head 2 months ago
Patient was apparently asymptomatic 2 months ago then she had a h/o of taruma with lacerations over parietal region for which suturing was done,from then she had h/o of headache which was throbbing pain, continuous,non-radiating accompanied by burning sensation of eye and lacrimation of eyes.
No h/o blurring of vision
No h/o nausea and vomiting
No h/o seizures, diplopia
SYSTEMIC EXAMINATION:
Respiratory System
- upper respiratory tract : oral cavity, nose & oropharynx appear normal
- chest is bilaterally symmetrical
- respiratory movements appear equal on both sides and of thoracoabdominal type
- position of trachea : central
- vesicular breath sounds : present
-no wheeze
Cardiovascular System:
Inspection :
- shape of chest : elliptical
- no engorged veins, scars, visible pulsations
Palpation :
-Apex beat can be palpable in 5th intercostal space
- no cardiac thrills
Auscultation :
- S1,S2 are heard
- no murmurs
Abdomen:
- shape: obese
- no tenderness
- no palpable mass
- no bruits
- no free fluid
- hernias orifices: normal
- liver: not palpable
- spleen : not palpable
- bowel sounds:yes
- genitals: normal
- speculum examination : normal
- P/R examination : normal
Central Nervous System:
- conscious
- normal speech
- no neck stiffness
- no Kerning's sign
- cranial nerves: normal
- sensory : normal
- motor: normal
- reflexes: all present bilaterally
- finger nose in coordination: not seen
- knee heel in coordination: not seen
- gait: normal
-Skin:Scar on parietal region
INVESTIGATIONS:
Hemogram
Bleeding and clotting time
Urine examination
HIV 1/2Rapid Test
HBsAg-Rapid
Anti-HCV Antibodies -Rapid
USG
PROVISIONAL DIAGNOSIS:
Chronic headache secondary to post trauma USG of left foot showed 2mm hyperechoic foci noted in left plantar aspect,surgery was done foreign body is removed
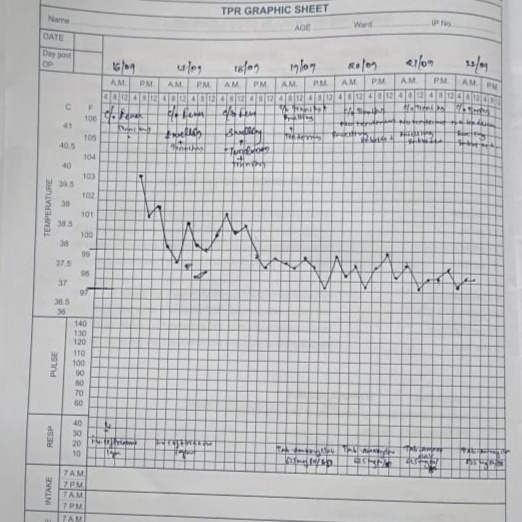
TREATMENT:
TAB.Paracetomol 40mg
TAB.HIFENAC-P
TAB.LIMCEE 500mg